Learning About Better Diagnosis Through People Living With Lupus
A Pulse patient safety advocate/instructor met with a small group of community residents who have been diagnosed with lupus at the Lupus Alliance of Long Island/Queens office in Bellmore, Long Island. Each person received their diagnosis at a different stage of their life, from as recently as a year ago to more than 10 years ago.
 People who have been diagnosed with lupus agree that all cases, though similar in nature, may have very different symptoms. Some have more joint discomfort than others while some participants explained that their skin was very sensitive to sunlight and they needed to be covered up in the hot sun or warm weather. Lupus is known to mimic other illnesses which may cause a delay in diagnosis. A clinician who is considering the possibility of lupus will look for signs of inflammation which include, pain, heat, redness, swelling, and loss of function at a particular place in the body. The clinician will look for abnormal blood tests, rashes, and extreme fatigue. Various immunosuppressive medications are used to treat these symptoms. Lupus may be treated by seeing specialists in the affected areas, such as rheumatologists, immunologists or nephrologists. Medication may be used to treat the symptoms.
People who have been diagnosed with lupus agree that all cases, though similar in nature, may have very different symptoms. Some have more joint discomfort than others while some participants explained that their skin was very sensitive to sunlight and they needed to be covered up in the hot sun or warm weather. Lupus is known to mimic other illnesses which may cause a delay in diagnosis. A clinician who is considering the possibility of lupus will look for signs of inflammation which include, pain, heat, redness, swelling, and loss of function at a particular place in the body. The clinician will look for abnormal blood tests, rashes, and extreme fatigue. Various immunosuppressive medications are used to treat these symptoms. Lupus may be treated by seeing specialists in the affected areas, such as rheumatologists, immunologists or nephrologists. Medication may be used to treat the symptoms.
All agreed that there is joint pain at times, and severe fatigue. There may be encouraging bursts of energy that allow the person to get more done, but then the cycle starts again. The participants in this focus group acknowledged that their immune systems may have been compromised and that they may get very sick when exposed to germs – making a hospital emergency room or physician’s waiting room an obstacle to safe care. The amount of time spent with their clinician was another concern in care. Participants felt that there was not enough time to go over their lists of symptoms. Communication breakdown also plays a role in quality time with lupus patients and their clinicians. The presentation started with introductions and then described patient safety issues: falls, infections, medication safety, health literacy, advance directives, and communication for the best diagnosis.
At different times throughout the program participants would describe what they might tell the clinician at an appointment about any pain or discomfort or fatigue. One woman said that people tell her they too are tired, but she explained that, “it’s not the same.”
Participants were asked to explain how they describe what they feel. We made a list of the “exaggerated” words. “So tired,” or “really exhausted” does not give an accurate description of how they feel. Taking the challenge to be more specific, one woman said “I was so tired, if you put a blanket on the floor I would lie down and go to sleep.”
Another told us that she is so tired she struggles to work and may not go to her job so she can rest.
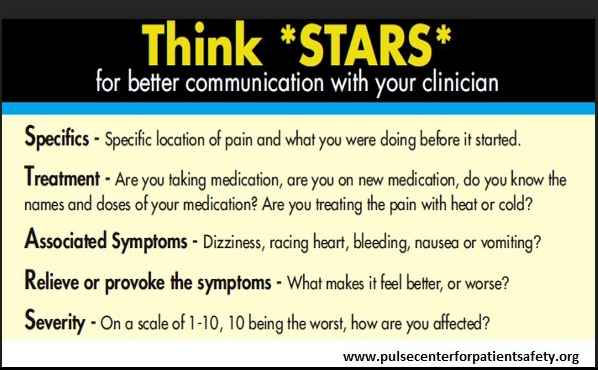
Using the STARS handout developed by Pulse, participants were asked to describe their symptoms more specifically. An example was used, that a woman’s leg hurts:
Specifics (specific location of pain and what were you doing before it happened) – My knee hurt when I stepped off the curb.
Treatment (are you taking medication or doing anything to treat the pain?) – I didn’t do anything for it. No ice packs, no heat.
Associated Symptoms (dizziness, nausea, bleeding) – Nothing else is bothering me.
Relieves or provokes the pain (what makes it feel better or worse?) – It only feels better when I am off my feet.
Severity – (On a scale of 1 to 10, with 10 the worst) — It feels like an 8 right now
Patient care can be improved by helping patients with lupus understand that it is their responsibility to help the clinician and their support system (family or friends) understand why their exhaustion is different from that of a woman who works a full time job and comes home at night to two young children. Healthcare professionals may need to help patients be more specific about symptoms and understand that they may not know the words to describe how they are feeling. Recommended follow up information should be developed and made available to people considering a diagnosis of lupus or already diagnosed, about how best to explain their symptoms — such as by using the STARS tool. Clinicians might use these examples in communication training and practice.
Resources
